I am very grateful to ENHPATHY consortium for giving me the opportunity to be part of this PhD project.
In my view, it is fascinating to understand how further genetic regulation may occur through chemotherapeutic drug stimuli that can increase the activity of specific enhancers.
In my PhD project I will be involved in studying genetic adaptations taking place after exposure to standard-of-care drug and their association to resistance in acute myeloid leukaemia (AML).
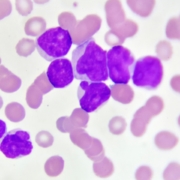
The AML is the most common acute leukaemia in adults. The disease is characterized by an uncontrolled clonal proliferation of undifferentiated myeloid precursor cells in the bone marrow and usually their presence in peripheral blood.
With a median age of 68, the World Health Organization (WHO) system divides AML into several groups:
- AML with recurrent abnormalities;
- AML with myelodysplasia-related changes;
- therapy-related AML;
- AML not otherwise specified.
Although the discovery of the most recurrent genetic mutations (i.e. FLT3-ITD, NMP1 and CEBPA) has certainly helped to provide better treatment support, to date the standard of care remains the intensive chemotherapy treatment with anthracyclines and aracytidine but with poor results. Indeed, responses are not durable, and majority of patients relapse with acquired drug resistance and die from the disease afterwards.
AML remains a clinical challenge and both a better understanding of the resistance mechanism and new therapies are urgently needed.
Doubtless drug resistance is related to the gravity of genetic mutations underlying AML, but it is also related to the alterations in the epigenetic regulation of proximal promoters and distal enhancers. In this field, a better understanding of the epigenetic regulation underlying resistance to chemotherapy treatment in AML could respond to the need for new therapies.
Accordingly, the main aim of this project is to study regulatory elements that are directly targeted by anticancer drugs in order to analyze in depth associated with drug resistance.
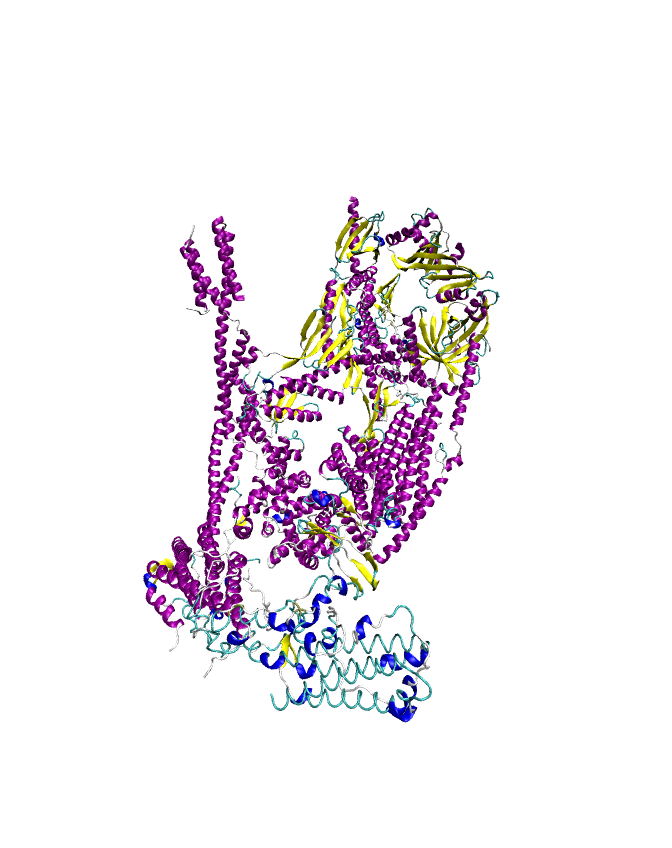
The human ALDH gene superfamily consists of 19 isoforms from 19 genes in 11 families and four subfamilies. Physiologically, the major function of ALDH enzymes is cellular detoxification via the NAD(P)H-dependent oxidation of toxic aldehydes into carboxylic acids. Aldehydes are produced naturally as by-products of the metabolism of glucose, amino acids and lipids, but also may come from exogenous sources like exposure to chemicals, including chemotherapeutic agents. Importantly, the oxidation of aldehydes is not the only catalytic function of ALDHs. Some members of the superfamily are known to have esterase or nitrate reductase activity and other various functions notably in cell differentiation and cell signalling.
Consequently, in cancer cells, where metabolic demands are elevated, and/or genetic mutations lead to an aberrant metabolism, the formation of endogenous toxic aldehydes is often exacerbated. In this contest, ALDH may represent a key survival adaptation and a marker of malignancy.
In particular, the ALDH subfamily 1A is associated with tumor progression and refractoriness and are elevated in multiple cancer types. These isoenzymes have been widely associated to poor prognosis, high tumorigenic potential and drug resistance.
In the context of AML, multiple studies suggest that ALDH1A1 is strikingly associated with drug resistance and increased risk of relapse.
Recent progress achieved by Advanced BioDesign (ABD) have shown that higher ALDH1 activity is characteristic of leukemic cells in refractory patients and in patients with adverse prognosis. More so, using different AML cells lines, they have found that certain chemotherapeutic drugs can modulate gene expression of at least three closely related isoforms of the ALDH family associated to drug resistance, thus supporting the idea of this project.
Currently, ABD develops specific inhibitors against ALDHs. The anticancer activity of these compounds has been demonstrated in prostate, non-small cell lung cancer and melanoma and more recently in preclinical models of AML.
The specific objectives of our project are:
- To map enhancer or promoter regions that are disturbed in AML and normal hematopoietic cells during anticancer drug exposure (namely, Daunorubicin, DIMATE and Ara-C) and identify their putative target genes.
- To characterise the role that the identified regulatory regions have in drug resistance.
- To assess the ability of the most prominent factors to sensitize or re-sensitize AML cells to undergo programmed cell death.
We expect to:
- identify the drug-responsive regulatory elements directly responsible for the severity of AML and their drug resistance traits;
- discover rational strategies with improved therapeutic efficacies by targeting enhancers with inhibitors that can modulate the transcription of the genes linked to drug resistance.
I hope you enjoy my blog, and I am looking forward to sharing with you my first results.
Francesco.